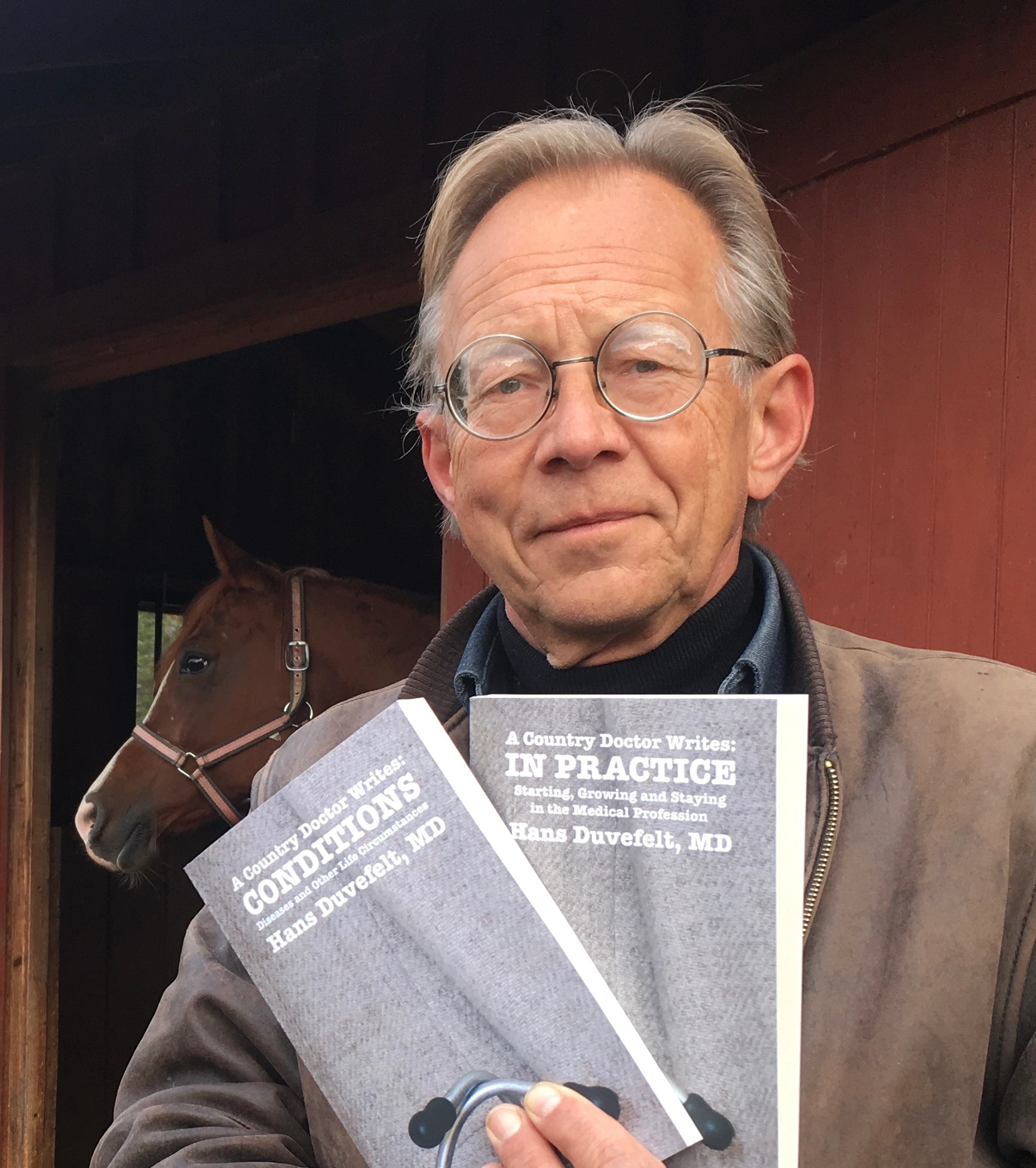
The Last Book I Brought Home From Medical School (I was an Editor): Terapikompendium
Published March 3, 2026 Progress Notes Leave a CommentRummaging through medical textbooks and notebooks from medical school in my library the other day I rediscovered a compendium that I had almost forgotten. I was one of the editors of this 256 page down and dirty guide for what to do when starting your internship. After I moved to this country, I learned that there already was such a book over here, called the Washington Manual. But back in Sweden in 1979, I was one of the editors or what we should have called the Uppsala Manual.
In Sweden, you can work as a physician, although under supervision, during the last two years of medical school and many of us had done that in different specialties. I had worked in nursing homes and in urgent care. My urgent care shifts were in a side wing of a small emergency room a short distance from Uppsala, where I lived. My shift started Friday 6 PM and ended Monday morning 6 AM. The triage nurses would decide which patients needed to see the emergency room for all the services they offered and which patients could be seen in the urgent care clinic next to it.
I loved that job.
Many of us in my medical school class got together to create an intern’s pocket size reference guide for what to do in common situations. This was based on what we learned in medical school and what we learned in our early practice positions. After I moved to this country, I found that there were a few similar books published by commercial publishing companies here, but there was no such thing available in Sweden when we graduated from medical school in 1979.
Looking at this book today, there are some striking differences in approach, partly based on evolving understanding of disease processes and also, of course, because of new imaging possibilities and new pharmaceuticals to treat disease.
In a future post I will give some examples that may seem quaint or even odd reading them now, 45 years later.
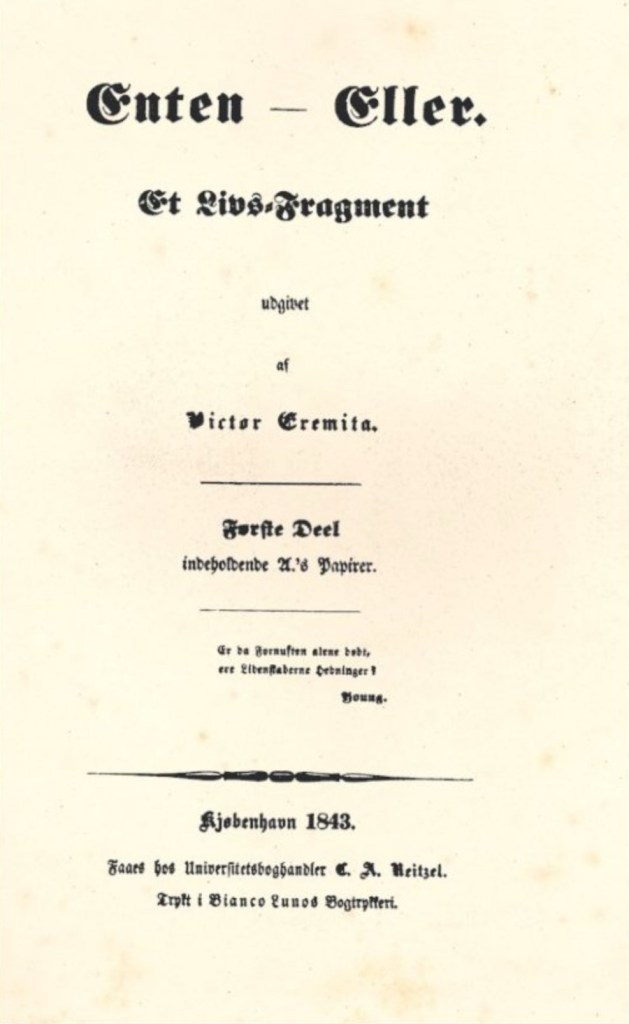
First, a side comment about languages. I was taught British English and there, a T is a T and a D is a D, but in American English that distinction is minimal. So this headline, when spoken, could easily give the illusion that I ride horses. I have horses, but I just keep them and spoil them, I do not ride them. But that is a side issue. The relevance here is that since I was sick most of February with a little horse farm, I still had to do all the heavy manual labor that goes with it.
I did not get much writing done during February because of my prolonged influenza (in spite of my vaccination) and its slow recovery. I was not able to fully disengage from my work during my illness because we are a fairly lean outfit here in Maine. That took a lot out of me.
So please accept my apologies and know that I have several pieces percolating and started that will be published in the coming days.
So I did not fall off the face of the earth, and I did not lose my desire to share my experiences and reflections as a country doctor in this fairly remote area. Stay tuned.
Kierkegaard’s Either/Or: A Prelude to Nietzsche’s Beyond Good and Evil
Published February 12, 2026 Progress Notes Leave a CommentI listened to a couple of Blinkist book summaries tonight. Even though I knew of Kierkegaard as the father of existentialism, I did not understand that there was some humor and humanity in his writings.
His first major work, published 1843 in Danish under the pseudonym Victor Eremita (suggestively similar to the Danish word for hermit, eremit), was titled Enten/Eller, Either/Or.
It contrasts aesthetic, his word for hedonistic, versus ethical views of life and states neither is all good, and whatever we choose, we will have to deal with the anxiety of our choices. The hedonist tries to escape their guilt by more hedonistic acts while the ethicist feels anxious by whatever degree of self-denial they have.
In the end he points out that the human condition is messy and unfair and we have to accept its unfairness and absurdity with a sense of humor.
I was surprised by his claim that living an ethical life would create anxiety. It’s easier for me to see that hedonism can lead to anxiety and attempts to sink deeper into their pathology (which Nietzsche saw as the new way of ruling the word). Link to my piece about that below. Meanwhile, I’m thinking of writing about anxiety and my lack of it on my personal Substack soon.
Beyond Good and Evil: Nietzsche Foresaw the Übermenschen of Today
Medicare Denial of Oxygen: I wasn’t Stupid, Just Ignorant
Published February 5, 2026 Progress Notes Leave a CommentI got an ominous looking fax in my electronic inbox today. WellCare was notifying me that my oxygen dependent COPD patient’s concentrator rental was going to be terminated because her “plan limit for home oxygen rental is 36 months. You have used 36 months rental of this service and would be eligible for new equipment 3/22/28 if needed”.
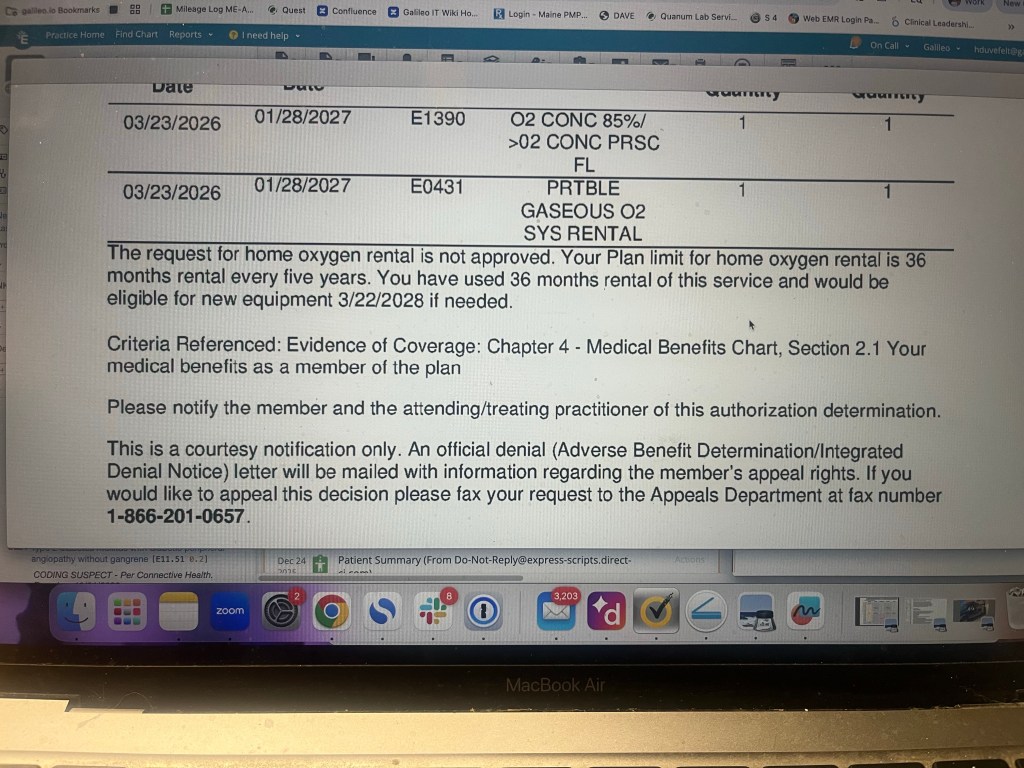
It was 10 minutes before 5 on this Thursday afternoon. I called the oxygen company and they answered in a cryptic way “Medicare only pays for 36 months, that is correct“.
“So what do people do“, I asked, “go without? Die?”
“We don’t take their equipment away“, the woman at Lincare said.
“You just don’t get paid then”, I asked.
“Correct“, she answered.
I love it when I learn something new about the practice of medicine. But most of the time when I learn a new aspect of how the “system” works, it just feels bewildering because it makes no sense. Wouldn’t anybody think that the rent per month would go up so as to cover the service and maintenance during the 3 1/2 years that go by after the 18 months of Medicare payments stop?
I once had a separate WordPress blog, and I think im still paying for the domain ”A Country Doctor Reads”, where I wrote bout my eclectic reding, not only from medical journals, but also from major news media, business journals and even Swedish newspapers. I later made it a post category here on A Country Doctor Writes.
It occurred to me to check if today, here and now, there is any interest in occasional posts on this theme. Comments are welcome. Check out this example from 2019:
A Country Doctor Reads: January 13, 2019