Substack is enhancing their video capabilities. I’ll be posting more videos there soon. Topics in the immediate pipeline are Atrial fibrillation, tuning fork testing for hearing loss and more, pinhole in a piece of cardboard for advanced eye diagnosis and more things to do with a blood pressure cuff. Follow me at ACDW.Substack.com or Acountrydoctorwrites.com.
Archive Page 20
Substack is a bigger platform that gets me much more exposure than my own little corner of the Internet. I have been re-posting old material there with lots of views. This one is from 2014:
“Prior Authorizations, Mrs. Kafka. May I have your name and the patient’s policy number.”
“My name is Country Doctor, and I don’t have the patient’s number but I have her husband’s – it is 123456789”.
“Thank you, Doctor. This is for Harry Black?”
“Well, no, it’s for his wife, Harriet. We asked for a PA for Lyrica for her, but it was approved for him instead, even though the forms we sent you clearly stated her name.”
“I see that Harry is approved for one year.”
“Yes, but he doesn’t need it. He has no diagnosis and no symptoms. Someone at your end reversed the names, because the application was for Harriet. I have a copy right here in front of me. So can we just get this approval switched over to her name instead?”
“I’m sorry, we can’t.”
https://open.substack.com/pub/acdw/p/calling-mrs-kafka?r=254ice&utm_medium=ios&utm_campaign=post
On the Road and at Home in Maine: I Do House Calls
Published November 10, 2023 Progress Notes Leave a Comment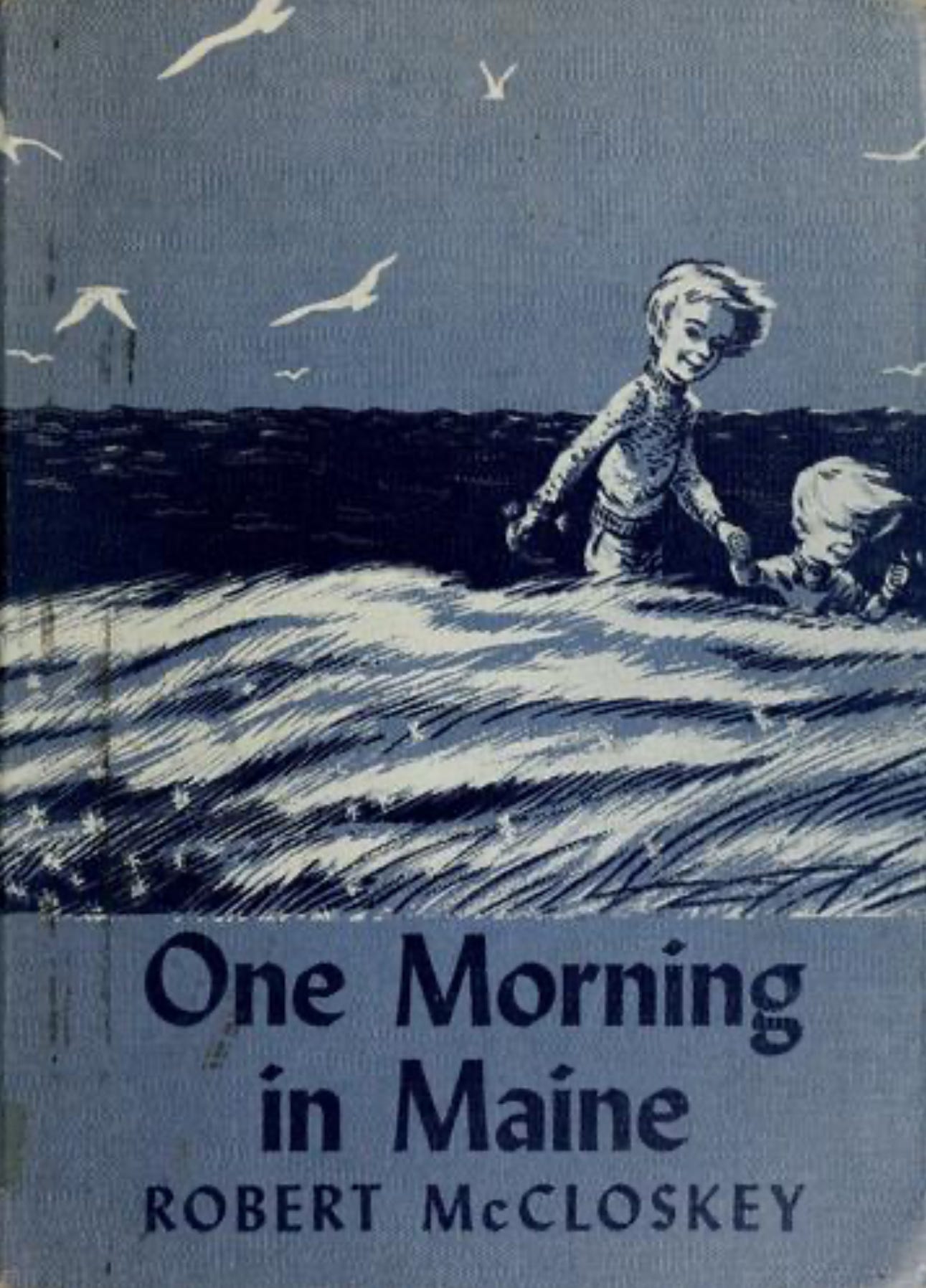
One Morning in Maine (that’s a famous children’s book, at least locally), I set off to my new office in Presque Isle. There is a fairly dense fog as I leave the house at 7:30. I usually don’t have to leave this early, but on this day I am scheduled for a mask fitting, with COVID still a close reality.
I didn’t want to go through Caribou in the morning traffic on Route 1 to Presque Isle with lots of stops for red lights, so I am following the Grimes Road along the northern shore of the Aroostook river to Fort Fairfield. As the fog slowly lifts, I see more and more of the river and the foliage. I pass Rocking S Ranch, where there are groups of boarded horses eating round bale hay in the nearly barren fields. My own horses probably wouldn’t eat round bale; I left them munching on second cut hay, an almost rare delicacy here in northern Maine.
Going from Fort Fairfield toward Presque Isle, I don’t turn right on my usual weekend shopping road that would bring me past Lowe’s to a fairly busy part of town, but continue past Amish country with more horses in the fields and some shackled to buggies standing outside the farm houses. In Easton I turn right and eventually pass the small hospital in Presque Isle and then turn onto a side street before I even see the very first traffic light on my journey and I actually arrive at the office in less time than if I had taken the busiest road through town.
My first house call for the day is an hour away, close to Houlton. I see Edwin Starks, a man with multiple medical problems and spotty medical care. Halfway through our one hour initial visit I know that he had been misdiagnosed and that he suffers from an iatrogenic condition (an avoidable disease caused by his previous providers’ misguided medication choices).
Read the whole post;
https://acdw.substack.com/p/on-the-road-and-at-home-in-maine










